What Patients Should Know About Quadriceps sparing and outpatient knee replacement
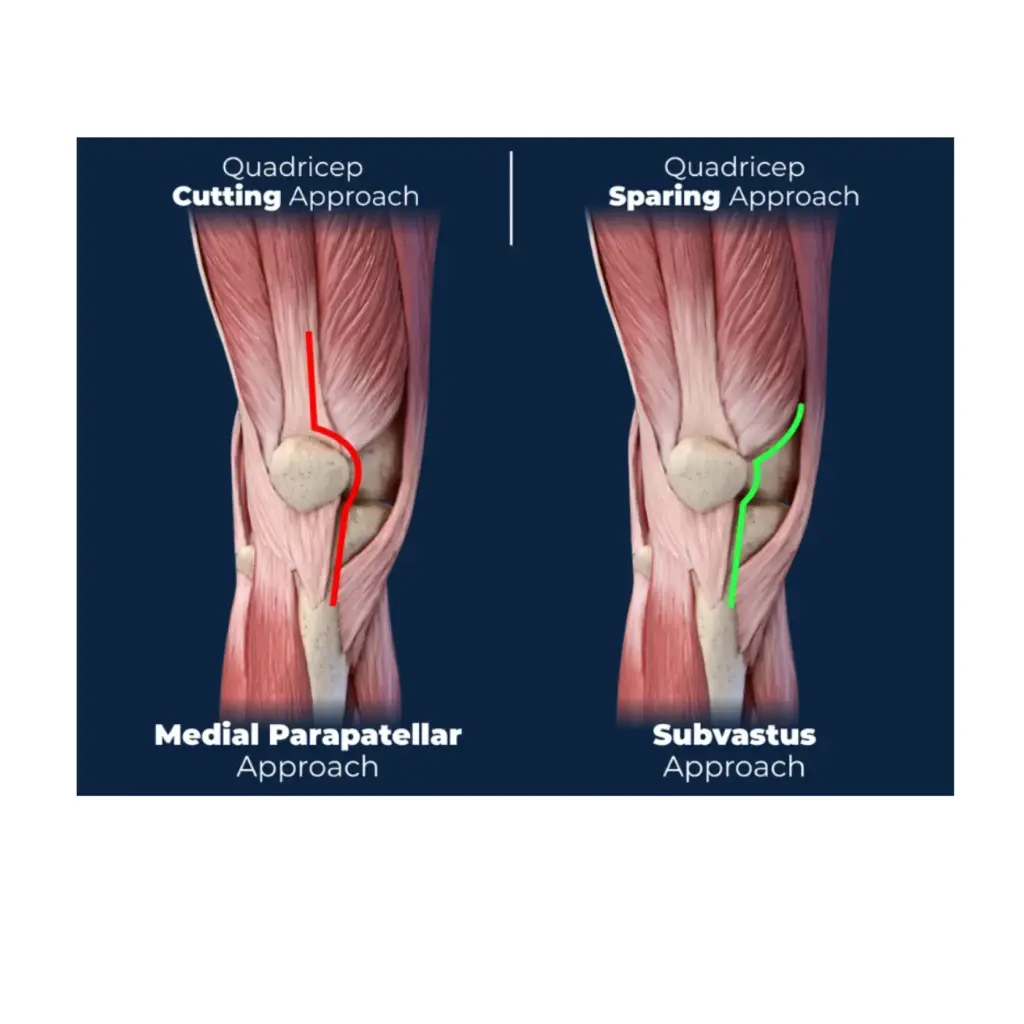
Medial Parapatellar Approach
This is the most commonly used approach in traditional total knee replacement. The incision goes through the quadriceps tendon and reflects the kneecap to access the joint. It provides excellent visibility for the surgeon but also involves:
● Cutting through the quadriceps tendon
● More trauma to surrounding soft tissue
● Longer time to regain normal walking and stair climbing
Subvastus Approach (SubV)
This technique avoids cutting the quadriceps tendon. Instead, the surgeon works underneath the vastus medialis muscle—hence the term subvastus.
What that means:
● No cutting of the quadriceps tendon
● Muscle-sparing, or quadriceps-sparing
● Potential for less pain and faster early recovery
If you would like to schedule a consultation with Dr. Appell, please call (205) 397-5200 or book an appointment online.
/
Other Names Patients Might See for the Subvastus Approach
Here’s where the confusion often grows. The subvastus approach can go by several names, especially when practices or surgeons market their own brand of minimally invasive surgery. No matter the name ascribed to the procedure, it is all the same technique with small variations.
Terms you might hear include:
● SubV Knee
● SubVy Knee
● Subvi Knee
● Suby Knee
● Suvi Knee
Which do you like the best?
These are not different techniques. If you are trying to compare options, focus less on the brand name and more on these questions:
● Will my quadriceps tendon be preserved?
● Is this truly a subvastus or muscle-sparing technique?
● Is the procedure assisted with robotic or AI assisted navigation.
● Can this be done as an outpatient procedure?
How to Know If You Are a Candidate
Most patients with arthritis-related joint damage are strong candidates for this approach. It may not be appropriate for everyone. Patients who have had previous knee surgery or require revision may not be a candidate, but most everyone else is.
That is why I assess each patient individually using:
● Imaging
● Strength and flexibility exams
● Health history
Enhanced Recovery After Surgery
Dr. Appell and his team utilize an Enhanced Recovery After Surgery (ERAS) system developed by the ERAS Society to minimize opiate use, reduce recovery time and improve patient outcomes.
This begins with educating patients thoroughly to make sure they understand what their surgery entails, what to expect when they return home, and the general timeline for recovery.
- Spinal anesthetics allow Dr. Appell’s team to operate without narcotics.
- Propofol puts patients in a twilight stage.
- Spinal anesthetics last for two hours so that patients don’t wake up in pain.
- Eliminating narcotics eliminates the post-op nausea and vomiting that has prevented people from going home post-surgery.
Post-surgery pain management:
- A nerve block injected into the knee reduces pain for 48 to 72 hours after surgery.
- Nerve medication, Tylenol, and non-steroidal anti-inflammatory drugs (NSAIDS) limit the need for opiates.
- An icing machine, connected to a wrap that encircles the leg, pumps ice water around the knee to reduce swelling.
Partial Knee Replacement in the Birmingham, Alabama
Dr. Scott Appell, a board-certified orthopedic surgeon, is one of the first surgeons in Alabama to use the Oxford partial knee system, considered to be the gold standard for partial knee replacement because of its mobile bearing, which has been shown to have greater longevity than those with a fixed bearing. Close to 25% of his knee replacement patients qualify for this less invasive, partial knee option, and he has done more Oxford knee procedures than anyone in the state. If you would like to schedule a consultation with Dr. Appell, please call (205) 397-5200 or book an appointment online.
